Managing challenging situations
Throughout their career, chiropractors will inevitably encounter challenging situations. This is to be expected when working with people to provide care and when interacting with individuals who hold different values and priorities than you. The resources below are adapted from Physiotherapy Alberta and are meant to assist chiropractors as they navigate challenging situations.
- Overview
- Why do challenging situations arise?
- Steps to follow if you are in a challenging situation
- Other potential sources of conflict
- The decision cycle
- Components of effective working relationships
- Conclusion
- Appendix A: reporting to authorities - what does the law say?
- Appendix B: what to do when there isn't a positive duty to report
- Appendix C: the DESC and modified DISC responses
- Appendix D: the BLAST technique
- References
Overview
What is a challenging situation?
Anything that interferes with a chiropractor’s ability to deliver quality patient care. Although the nature of the situation can vary, it is very likely that chiropractors will encounter challenging situations over the course of their career. This resource is meant to support chiropractors when dealing with challenging situations with their patients, patient family members or other health-care providers. While that is the intended purpose for these resources, they can also be applied to any challenging situation.
Challenging situations can arise from interpersonal conflicts like differences in values or expectations, availability of health-care resources or other factors. Different personalities can also contribute to how challenging a situation is. Regardless of these factors, chiropractors are in a position of authority and are expected to maintain a professional and respectful manner when managing challenging situations.
While these situations can cause concern for patients and chiropractors, it is important to remember that most interactions with patients will be positive. When conflicts do arise, they are often manageable with clear communication, expectation setting and clarity on values and priorities. This approach demonstrates patient-centred care.
The continuum of challenging situations
It may help to think of challenging situations as being on a continuum. While most situations can be managed with effective communication and clear expectations, some situations are more complex and thus, harder to manage.
How to use this guide
This guide outlines why conflicts arise, components of effective relationships, and introduces some communication and conflict management techniques.
If you are currently experiencing a challenging situation, follow these steps.
Why do challenging situations arise?
Conflicts or challenges can occur for a multitude of reasons, including difference in values, assumptions or expectations between individuals. Although challenging to maneuver, conflict is a normal and predictable part of human interaction. The challenges you face will differ depending on the situation, as will your strategy for dealing with them.
Take the time to reflect on your own beliefs and values, and be proactive in doing the same for your clients. By doing this, you can set clear expectations and avoid conflict. If you still encounter conflict, try to view it as a learning opportunity to develop new skills. This way of thinking may help you view a negative situation in a more positive light.
Challenging situations can sometimes arise between health-care providers or between chiropractors and a patient’s family member. When dealing with these kinds of conflicts, remembers that in addition to differences in values, assumptions and expectations, there is often other elements at play too—such as differences of influence or hierarchy, knowledge or perception. When conflict exists between the chiropractor and a patient’s family, issues such as the family’s desire to advocate for their loved on and their need to be valued for their contribution can also be factors in conflict. It’s important to remember in these situations that as a health-care professional, you are expected to demonstrate respect and professionalism when addressing conflict.
There are many resources available that discuss communication and conflict management theories. Appendix C and appendix D provide two models that may help you in your practice.
Some examples of challenging situations chiropractors may encounter in practice include:
- Patients uttering threats.
- Patients expressing suicidal thoughts.
- Situations where public safety may be at risk (patient drove intoxicated).
- Conflicts with patient family members.
- Meeting specific contractual obligations such as reporting to WCB when a patient does not want you to.
Steps to follow if you are in a challenging situation
If you find yourself in a challenging situation here’s a step-by-step process for how to proceed:
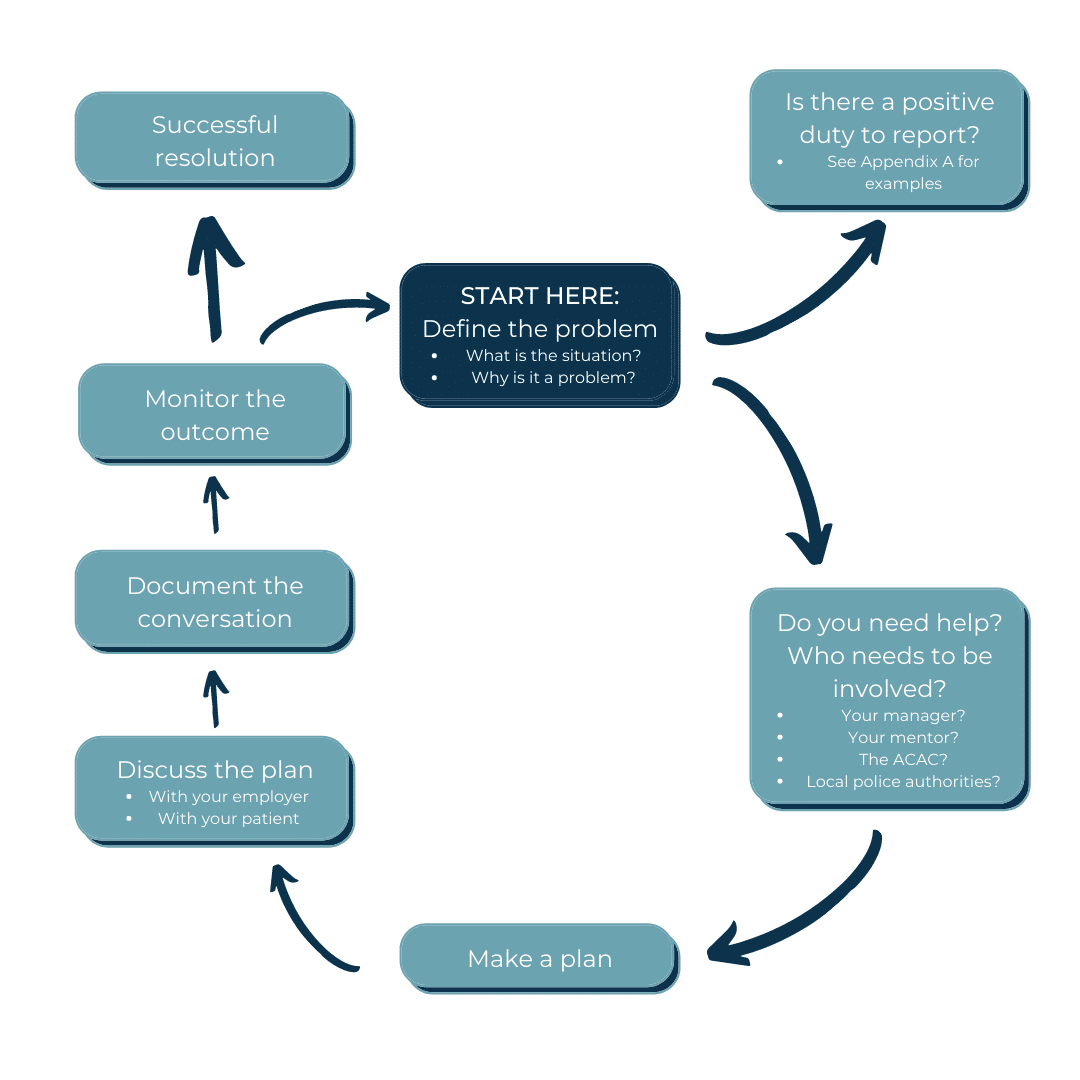
- Define the problem. What exactly is the situation? Why is it a problem? Take a moment to reflect on how your own values, beliefs and experiences are influencing the problem. Consider what the other person’s values, beliefs and experiences may be.
- How severe is the problem? Do you need to get help from your manager or from an outside resource to safely and effectively manage the situation?
- Does the situation result in safety issues for the patient, the chiropractor or the public? Do you have a positive duty to report the situation to the authorities? See Appendix A for specific examples of situations where you are legally required to report a situation to authorities.
- What do you want from your discussion? What sort of resolution are you hoping for? Knowing what you want before starting the conversation increases the likelihood of an outcome that you desire.
- Plan the conversation. The balance of power in a patient/provider relationship rests primarily with you and therefore so does the responsibility to resolve the issue. Even if the conflict doesn’t involve a patient, the onus is on you as a professional to address conflicts appropriately. Consider what you are going to say (make a script if you need to). Schedule a meeting with the other person to discuss the issue or set aside extra time at their next appointment. Even if your employer isn’t directly involved in managing the situation, it is a good idea to let them know your plan, especially if the person’s behavior is severe or you have concerns for your safety.
- Discuss the situation. Listen actively to the other person’s perspective.
- Document the conversation and your plan for managing the situation.
- Monitor the results of your conversation. Did the issue resolve? If yes, congratulations! If not, consider repeating the cycle, getting help from your employer or contact the CCOA for guidance.
- Reflect on the situation. What could you have done differently to manage things? Are there any changes you would make to your routine practices or communication with patients that would help to avoid a similar conflict in the future?
Positive duty to report
A positive duty to report means that you are legally required to report the behavior/situation to the appropriate authority as soon as you become aware of it. This includes breaching the confidentiality of the patient’s private information to make a report. In these situations, a failure to report can result in you being fined for not fulfilling your legal responsibilities. For examples of when a positive duty to report applies, see Appendix A.
Other potential sources of conflict
Family members
There are important considerations to keep in mind when family members are actively involved in the care of a client. First, is the patient able to make their own decisions? If yes, then they should do so and all questions about care should be directed to them. It is also necessary to determine to what extent the patient wants their family member involved in their care, patient education and treatment planning.
In the event that an adult patient is unable to make their own decisions, the chiropractor needs to establish who has the authority to make decisions on the patient’s behalf and direct treatment related decisions to that individual. When working with minors, it is equally important that you establish who is legally able to make decisions on behalf of the minor and who has the right to access information about the minor.
Establishing who can and should be involved in the patient’s care and the limits of that involvement, should be done at the onset of the therapeutic relationship.
Other health-care providers
Conflict can arise with colleagues as well, whether they are other chiropractors, other health professionals or others within the work environment. Many of the same skills and techniques of establishing good working relationships can also be used to manage and develop these professional relationships.
Health-care environments are traditionally hierarchical in nature, however when hierarchy prevents effective communication and working relationships it can lead to patient safety incidents. In fact, it has been estimated that 70 per cent of all patient harm incidents are caused by communication breakdown. All health-care workers have a responsibility to maintain positive working relationships with colleagues to facilitate safe care and healthy work environments. One way to achieve this is to seek ways to decrease the sense of hierarchy or power imbalance between you and those with whom you work. This can be achieved through simple behaviours like calling each other by first names, making eye contact and seeking input from everyone, regardless of their role in the organization.
The decision cycle
This decision cycle below is intended to help you decide what steps to take when working through a challenging situation. Consulting with trusted colleagues, your employer or mentors may also be helpful. In some cases, the most appropriate course of action is to have your employer involved in helping to resolve the situation.
Components of effective working relationships
As the chiropractor, it is your responsibility to manage challenging situations, which is why it’s important to know how to effectively resolve them or avoid them altogether.
The components of a good working relationship include:
- rationality
- understanding
- communication
- reliability
- non-coercive influence
- acceptance
- rationality
When establishing any working relationship, it’s important to consider your own values, beliefs and expectations. This will help you to identify your own personal frustrations and identify potential conflicts when working with clients and others.
Understanding
You also need to understand your client’s beliefs, values and expectations. Take a moment to think about how you would feel if you were in your client’s position and acknowledge their emotions. Begin with the assumption that you need to know more. It is not required that you share the same values or beliefs to work well together. It is required that you accept and acknowledge the other person’s values, treat them as an equal and demonstrate respect.
When you cannot meet the client’s expectations (for example due to funding or time limitations), it is best to discuss the situation as soon as possible. Similarly, if your employer has policies about billing for missed appointments or providing treatment when patients are late for appointments, conflict can be avoided or minimized by discussing the policies early in the relationship before issues arise.
By establishing expectations that you are sure you can meet, and applying a philosophy of “under promise, over perform” you will increase your chances of avoiding conflict.
If however you choose to tolerate situations arising from a patient’s unrealistic expectations or inappropriate behavior by hoping the patient’s behavior will change or the patient will cease treatment, you are not actively managing the situation and are not meeting the expectations for chiropractors in Alberta.
Communication
There are many resources available to support professionals who wish to improve their communication skills. The DESC method of assertive communication (Appendix C) and the BLAST technique for complaint resolution (Appendix D) are two such examples.
Basic principles of effective communication include:
- Practise active listening.
- Focus on the issue rather than the individual.
- Limit comments to the issue at hand, rather than past conflicts.
- Avoid the words “always” and “never.”
- Monitor both your verbal and non-verbal communication.
- Use humor cautiously, respectfully and never at the expense of the other individual.
Reliability
In many situations, inconsistent behavior can be more of a challenge than predictably poor behavior. When building working relationships, strive to model behavior that is:
- predictable
- clear
- honest
- Takes promises seriously.
When seeking reliability from others, remember to give trust when it is deserved and approach problematic behavior as a joint problem, asking “how do we fix this?”
Non-coercive influence
Remember that your focus is not on winning an argument, but on developing a better understanding of the patient and their perspective and settling on a new consensus about the best course of action. In clinical situations, it is rare that there is a single best course of action. The principles of evidence-based practice require that a combination of research evidence, clinical knowledge and patient preferences are used to inform treatment decisions. The best course of action for any given patient is not always the gold standard of care, but rather the best possible combination of all three sources of knowledge.
Remember that because of your knowledge, skills and role in the relationship, you are in a position of power. It is important that you work to decrease any power imbalances that exist between you and your patient, their family or other health-care providers by paying particular attention to what the patient’s preferences are. In doing so, you support patient-centered care and self-management, leading to better long-term patient outcomes.
Acceptance
Acceptance does not require that you agree with others’ values or approve of their conduct. It does mean that you treat others with respect and as equals and acknowledge that their views or values are what they are.
When you can’t build an effective relationship
There are times when it is appropriate for a chiropractor to discontinue treatment even though a patient wants and needs continued care. Physical, verbal, sexual or emotional abuse have no place in a therapeutic relationship. If a chiropractor perceives that they are at risk or are being abused by their patient, they have the right to decline to continue to provide treatment.
Chiropractors who are aware or made aware that their employees are at risk or are being physical, verbal, sexual or emotional abused by a patient attending in the office also have a duty to act for the employee’s safety. This is a circumstance where the chiropractor as an employer (where applicable) should be involved in resolving the situation. The Alberta College and Association of Chiropractors expects that employers will create and maintain healthy, safe work environments for their employees. This expectation extends to both physical and psychological hazards.
If the chiropractor is discontinuing treatment, the Code of Ethics (article A10) require that the chiropractor (or his/her employer) discuss the situation with the patient, explain their decision, provide the patient with a list of other sources of similar treatment, and (when possible) assist the patient to find alternate treatment providers. Depending on the situation, it may be appropriate for the chiropractor to provide a limited number of treatments until the patient can commence treatment elsewhere.
Conclusion
No one likes being in challenging situations. They are stressful and can often leave professionals feeling uncomfortable or uncertain of their decisions. Remember, nearly every situation offers the opportunity for learning. It’s important to engage in reflective practice and ask yourself if you can carry your new learnings forward for handling similar situations in the future.
Once a challenging situation has been resolved, it is important to take the time to reflect on one’s own values and beliefs and how these may have impacted the therapeutic relationship and the situation itself (for better or for worse). Sometimes situations within a chiropractor’s personal life may lead them to over-personalize a challenging situation. If the challenging situation has left you feeling emotions such as anger, guilt, shame or embarrassment, these feelings can cloud professional judgment and negatively impact other professional relationships.
It is important for chiropractors to take some time to process these emotions, reflect upon how they managed the situation and what they would do differently when faced with such a situation again. This may include seeking outside help from a supervisor, mentor or health-care professional if they are having difficulty coming to terms with the situation and its outcome.
Appendix A: reporting to authorities – what does the law say?
Although not every challenging situation will come with legal considerations, there are several laws that are relevant to chiropractors depending on the situation. It is important that chiropractors are aware of the broader ramifications of these situations and the actions they are legally required to follow when managing the situation.
| Example | Law | Requirements |
| The patient is intoxicated at his/her visit. The chiropractor doesn’t treat the patient. The patient leaves and the chiropractor is aware that the patient is driving while intoxicated. | Traffic Safety Act |
|
| The patient has a history of previously controlled seizures but has recently been having seizures again. The chiropractor is aware of the patient’s seizures. | Traffic Safety Act |
|
| The chiropractor suspects that patient, a dependent adult, is being mistreated by a caregiver. | Protection of Persons in Care Act |
|
| The chiropractor suspects that patient, a minor, is being mistreated by their parents. | Child, Youth and Family Enhancement Act |
|
| The patient reports that he/she is planning to commit suicide. The patient asks the chiropractor to not tell anyone. | Privacy Law: Personal Information Protection Act (PIPA) or Health Information Act (HIA) depending on the work environment. | |
| The patient expresses his/her intent to harm another individual. | Privacy Law: PIPAor HIA depending on the work environment. |
|
| The patient reports that they were injured at work but requests that the chiropractors not report the injury to WCB. | Workers’ Compensation Act |
|
Appendix A: reporting to authorities – what does the law say?
In cases where legislation does not require you to report concerns to authorities, there may still be an ethical or moral imperative that leads you to contact the authorities. When there is not a positive duty to report, the chiropractor must use their judgment to determine whether to report their concerns. In this situation you need to balance the potential consequences of not reporting the situation against the serious nature of breaching a patient’s privacy. In these circumstances the test for determining the need to report is as follows:
- The chiropractor perceives that there is a clear risk of harm to the patient or any other clearly identifiable individual.
- The danger poses a risk of serious bodily harm or death.
- The danger is imminent* (i.e., “a sense of urgency must be created by the threat of danger”).
When all three requirements are met, legislation allows a breach of privacy without patient consent for the purpose of alerting the appropriate authorities.
For example, in cases where the patient is expressing suicidal thoughts, privacy legislation permits the therapist to breach patient confidentiality to report their concerns. The therapist needs to determine the most appropriate person to report the situation to. The most appropriate person may be a family doctor, another health-care provider who works with the patient, a family member or guardian, or the local police authority.
Similarly, when an individual is expressing the intent to harm a third party, the chiropractor must use his/her judgment to determine whether to report this information and to whom. The same three requirements are applied to determine if disclosure without consent is acceptable.
Regardless of the actions they take, the chiropractor must endeavor to maintain a therapeutic relationship with the patient by offering support and acting in the patient’s best interest, in keeping with the CCOA Code of Ethics.
* While the relevant legislation indicates that the danger must be imminent. This does not mean that the action be occurring immediately. “The risk could be a future risk but must be serious enough that a reasonable person would believe that the harm would be carried out.”
Overview
These models provide a framework for handling any interaction where an individual needs to express their point of view. The DESC format is used when there is an established relationship with the other party and some confidence that the other party will respond in a mature, respectful manner.
In some situations there is greater risk and less certainty about the response from the other party. In this case, the E is replaced with an I for indicating the problem the behaviour is causing.
Describe
Describe the situation
Express/Indicate
Express your feelings about the situation “I feel …” or indicate the problem the behaviour is causing.
Specify
Specify the change you want. “I’d like you to …”
Consequences
identify the results that will occur. “In that way …”
The BLAST technique is use for complaint resolution. It stands for Believe, Listen, Apologize, Satisfy and Thank.
The BLAST technique
Believe
Express your belief in the truth of the patient’s concerns and the validity of his/her emotions, even if you do not agree with the legitimacy of them.
Listen
Use active listening to determine what the patient’s concern is and what his/her unmet expectations are.
Apologize
An apology is not always an expression of responsibility. However, if the complaint is legitimate, patients deserve an apology. Even if the complaint isn’t legitimate, they will expect one. By relating the apology to the patient’s unmet expectations you acknowledge their experience, even if you don’t perceive the complaint as legitimate.
Satisfy
Strive to satisfy the patient. Ask what the patient wants, to ensure you haven’t mistakenly assumed you know what he/she desires. Start by addressing any complaints or demands that you cannot meet. If the patient’s requests are reasonable, agree. If not, calmly explain why and propose some other options.
Thank
Thank the patient for sharing his/her concerns with you.
References
All information has been adapted with permission from Physiotherapy Alberta.
- Porter-O’Grady T. Embracing conflict: Building a healthy community. Health Care Management Review 2004; 29(3): 181-187.
- McFarlane, L-A. Trials and Triumphs: Working with challenging students. Lecture presented at The Collaborative for Scholarship in Clinical Education, Clinical Educator Workshop; 2015; University of Alberta.
- Rosenstein AH, O’Daniel M. A survey of the impact of disruptive behaviors and communication defects on patient safety. The Joint Commission Journal on Quality and Patient Safety 2008; 34(8): 464-471.
- Government of Alberta. (2014). Traffic Safety Act. Alberta Queen’s Printer. Available at: http://www.qp.alberta.ca/documents/Acts/t06.pdf. Accessed on June 9, 2015.
- Government of Alberta. (2010). Protection for Persons in Care Act. Alberta Queen’s Printer. Available at: http://www.qp.alberta.ca/1266.cfm?page=P29P1.cfm&leg_type=Acts&isbncln=9780779749904&display=html. Accessed on June 9, 2015.
- Government of Alberta. (2014). Child, Youth and Family Enhancement Act. Alberta Queen’s Printer. Available at: http://www.qp.alberta.ca/documents/Acts/c12.pdf. Accessed on June 9, 2015.
- Government of Alberta. (2014). Personal Information Protection Act. Alberta Queen’s Printer. Available at: http://www.qp.alberta.ca/documents/Acts/P06P5.pdf. Accessed on June 9, 2015.
- Government of Alberta. (2011). Health Information Act: Guidelines and practices manual. Alberta Queen’s Printer. Available at: http://www.health.alberta.ca/documents/HIA-Guidelines-Practices-Manual.pdf. Accessed on May 29, 2015.
- British Columbia Rehabilitation Society. Boundaries workshop materials. 1992.
- Davis, C. Patient Practitioner Interaction(4th ed). Thorofare: SLACK Incorporated, 2006.
- Steinman, H.K. A method for working with displeased patients—BLAST. The Journal of Clinical and Aesthetic Dermatology 2013; 6(3): 25-28.
- Alberta College and Association of Chiropractors Code of Ethics. https://albertachiro.com/legislation-and-standards